Nutrition and exercise are central aspects in the prevention of diabetes mellitus as well as in its treatment. Moving people are less susceptible to diabetes mellitus. Also less endangered are people who follow a healthy diet based on nutrient-dense whole foods.
For people with diabetes mellitus, lifestyle interventions that affect both diet and exercise are an optimal treatment alternative. This positively influences the risk factors (body composition, HbA1c value, blood pressure, insulin sensitivity, impaired glucose tolerance).
Prevention:
It is undisputed that moderate to intense physical activity is associated with a lower risk of developing type 2 diabetes (diabetes mellitus).
Chart 1 illustrates that particularly inactive individuals who add a certain amount of physical activity to their everyday lives benefit to a large extent. Generally, individuals with a high volume of moderate to intense physical activity have a lower risk of developing type 2 diabetes.
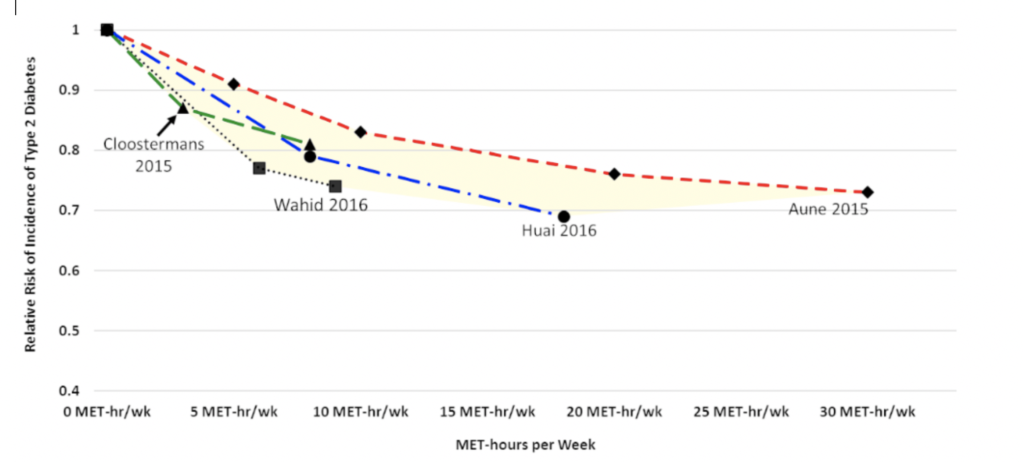
Chart 1: Relationship between the volume of physical activity and the relative risk of developing Type 2 diabetes. (Physical Activity Guidelines Advisory Committee Scientific Report, 2018)
Favorable dietary behavior in the prevention of type 2 diabetes is characterized by a reduction in refined carbohydrates, excessive starch, red meat, and added sugar, thus positively affecting blood sugar levels and insulin response (Ley et al., 2014). Red meat and sweet drinks, in particular, should be reduced, and carbohydrates should focus more on vegetables, salads, fruits and moderately whole grains (Chart 2).
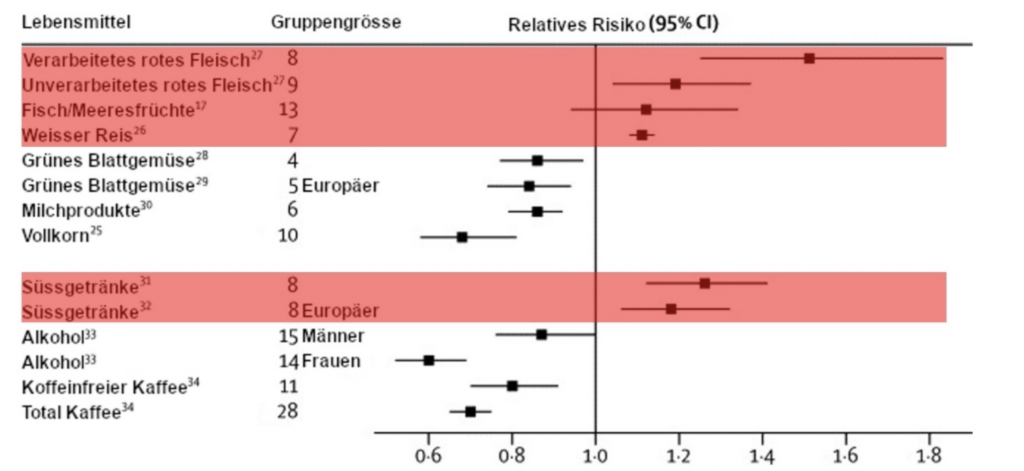
Chart 2: Relationship between diet and the relative risk of developing type 2 diabetes (Ley et al., 2014).
Disease progression:
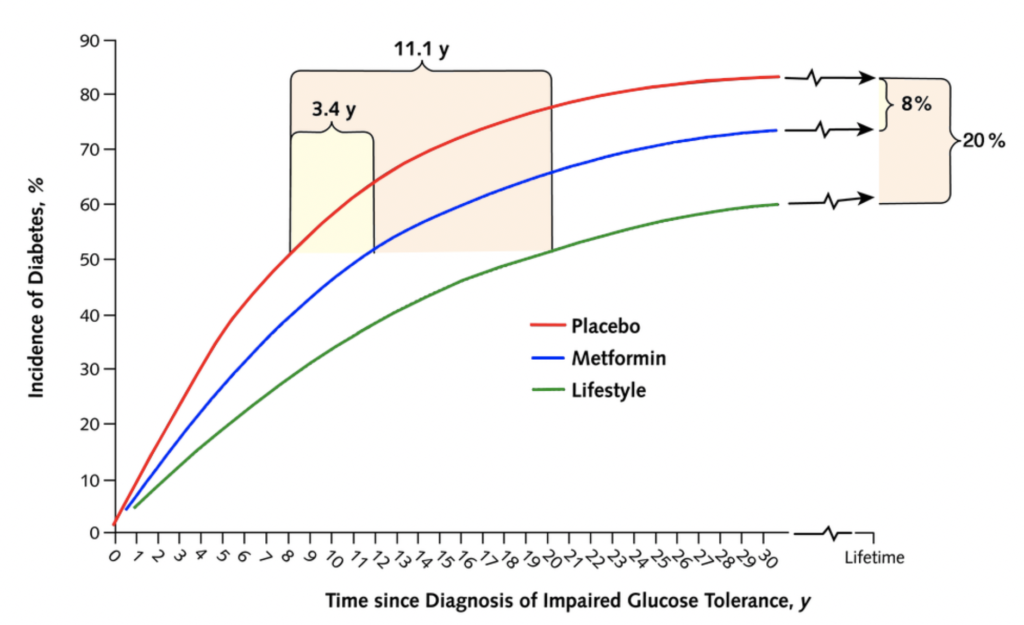
Physical activity also has a positive effect on the health of individuals who have already been diagnosed with decreased glucose tolerance. For many years there has been scientific evidence of the benefits of lifestyle intervention over drugs (metformin) and placebo intervention (see Chart 3). The onset of diabetes can be delayed by 11 years (lifestyle) or 3.4 years (metformin) versus placebo.
Chart 3: Simulated projected effectiveness of different interventions in individuals with impaired glucose tolerance to delay Type 2 diabetes (Herman et al., 2005)
Remission of Diabetes Type 2
In the best case, a Type 2 diabetes can also be reversed. Through more exercise in everyday life and a targeted nutritional adaptation in the direction of “low carb”, the energy balance can be controlled and thus effectively reduce the body weight over time. Scientific studies have shown that glucose levels in the blood can return to normal after a weight loss of 10-15kg of excess body weight in diabetics, reversing type 2 diabetes (Chart 4). This effect can be achieved in particular if this change takes place within the first few years after the onset of type 2 diabetes.
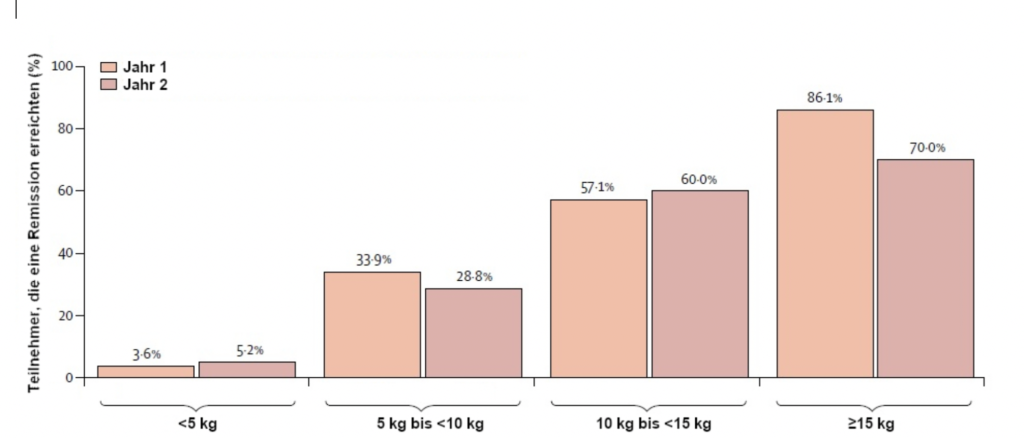
Chart 4: The greater the weight loss achieved by adaptive diet and exercise behavior in overweight diabetics, the greater the likelihood of natural remission of type 2 diabetes (Lean et al., 2019).
References:
Herman WH, Hoerger TJ, Brandle M, Hicks K, Sorensen S, Zhang P, et al. The Cost-Effectiveness of Lifestyle Modification or Metformin in Preventing Type 2 Diabetes in Adults with Impaired Glucose Tolerance. Ann Intern Med. 2005; 142:323–332. doi: 10.7326/0003-4819-142-5-200503010-00007
2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC: US Department of Health and Human Services; 2018.
Ley, S. H., Hamdy, O., Mohan, V., & Hu, F. B. (2014). Prevention and management of type 2 diabetes: dietary components and nutritional strategies. The Lancet, 383(9933), 1999–2007. https://doi.org/10.1016/S0140-6736(14)60613-9
Lean, M. E. J., Leslie, W. S., Barnes, A. C., Brosnahan, N., Thom, G., McCombie, L., … Taylor, R. (2019). Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. The Lancet Diabetes & Endocrinology, 7(5), 344–355. https://doi.org/10.1016/S2213-8587(19)30068-3
Disclaimer
The advice given above does not correspond to any medical advice nor does it describe a medical diagnosis or treatment method. All the information you find on Youdowell’s website, videos, blog posts, and other materials are just suggestions for you and possibly for your health care providers. The ideas, information and suggestions provided by Youdowell are not intended as a substitute for medical advice / care and you should not prefer the information in lieu of a doctor consultation or over the advice of health professionals. Youdowell AG is not liable for the ideas, content, references and suggestions provided.
